
Credit: John A. Rogers / Northwestern University.
Your skin is breathing. This wearable gas sensor can measure it.
Northwestern University researchers have developed the first wearable device for measuring gases emitted from and absorbed by the skin.
By analyzing these gases, the device offers an entirely new way to assess skin health, including monitoring wounds, detecting skin infections, tracking hydration levels, quantifying exposure to harmful environmental chemicals and more.
The new technology comprises a collection of sensors that precisely measure changes in temperature, water vapor, carbon dioxide (CO2) and volatile organic compounds (VOCs), which each give valuable insight into various skin conditions and overall health. These gases flow into a small chamber within the device that hovers above the skin without actually touching it. This no-contact design is particularly useful for gathering information about fragile skin without disturbing delicate tissues.
“This device is a natural evolution of our lab’s wearable electronic devices that collect and analyze sweat,” said Northwestern’s John A. Rogers, who co-led the study. “In that case, we were analyzing sweat to learn about the wearer’s overall health. While useful, that method requires pharmacological stimulation of sweat glands or exposure to a hot, humid environment. We started thinking about what we could capture from the skin that is naturally occurring all the time. It turns out there are all kinds of things coming off the surface of the skin — water vapor, carbon dioxide and volatile organic compounds — that can be correlated to underlying physiological health.”
“This technology has the potential to transform clinical care, particularly for vulnerable populations, including newborn babies, the elderly, patients with diabetes and others with compromised skin,” said Northwestern’s Guillermo A. Ameer, who co-led the study.
“The beauty of our device is that we found a completely novel way to assess the status of delicate skin without having to come in contact with wounds, ulcers or abrasions. This device is the first major step toward measuring changes in gases and correlating those changes with skin status.”
A bioelectronics pioneer, Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery at Northwestern — with appointments in Northwestern’s McCormick School of Engineering and the Feinberg School of Medicine — and the director of the Querrey Simpson Institute for Bioelectronics. Ameer is the Daniel Hale Williams Professor of Biomedical Engineering at McCormick, professor of surgery at Feinberg and director of the Center for Advanced Regenerative Engineering. Rogers and Ameer co-led the study with Yonggang Huang, the Jan and Marcia Achenbach Professor in Mechanical Engineering and professor of civil and environmental engineering.
Empowering patients at home
Called the skin barrier, the outermost layer of skin is the body’s first line of defense from the external environment. It maintains hydration by preventing excessive water loss and acts as a barrier against irritants, bacteria and ultraviolet radiation. When the skin barrier is compromised, it can lead to increased water loss (known as transepidermal water loss or TEWL), skin sensitivity, and risk of infection and inflammatory conditions like eczema and psoriasis.
“The skin is critical for protecting us from the environment,” said study co-author Dr. Amy Paller, the Walter J. Hamlin Professor of Dermatology and chair of the Department of Dermatology at Feinberg. “A major element of this protective function is the skin barrier, which is largely characterized by a formidable collection of tightly woven proteins and fats that keeps water in and irritants, toxins, microbes and allergens out.”
By tracking changes in the emission of water vapor and gases from the skin, health care professionals can gain a glimpse into the integrity of their patients’ skin barriers. While technologies to measure water vapor loss do exist, they are large, cumbersome machines that largely reside within hospital settings. The compact wearable device, on the other hand, is designed to help physicians monitor their patients remotely and to empower individuals to take control of their own skin health at home.
“The gold standard for measurement of skin barrier integrity is a large instrument with a probe that intermittently is touched to the skin to collect information about transepidermal water loss — or the flux of water through skin,” Paller said. “Having a device that can measure transepidermal water loss remotely, continuously or as programmed by the investigator — and without perturbing a patient during sleep — is a major advance.”
How the device works
Measuring just two centimeters long and one-and-a-half centimeters wide, the device comprises a chamber, a collection of sensors, a programmable valve, an electronic circuit and a small rechargeable battery. Instead of touching the skin directly, the chamber hovers a few millimeters above it.
“Traditional wearable sensors rely on physical contact with the skin, limiting their use in sensitive situations, such as wound care or for individuals with fragile skin,” Rogers said. “Our device overcomes this limitation by creating a small, enclosed chamber above the skin’s surface.”
An automatic valve opens and closes the entrance to this chamber — a function that dynamically controls access between the enclosed chamber and the surrounding ambient air. When the valve is open, gases flow in or out of the chamber, enabling the device to establish a baseline measurement. Then, when the valve rapidly closes, it traps gases within the chamber. From there, the series of sensors measure changes in gas concentrations over time.
“If our device didn’t incorporate a programmable valve and a time-dynamic measurement approach to quantify flux of species out of and into the skin in a real-time manner, then the system could be confounded by changes in the concentrations of these species that might naturally vary in the surrounding environment,” Rogers said. “Specifically, if the valve were open all the time, the sensor would detect these sorts of changes — not because of anything associated with the skin. On the other hand, if the valve were always closed, then it would perturb natural patterns of flux in a way that also could not account for environmental factors. For workers in potentially hazardous environments, it’s helpful to know how much of those hazardous species are entering the body through the skin.”
Ideal for wound care
Using Bluetooth, the device sends these data straight to a smartphone or tablet for real-time monitoring. These fast results can help health care workers make more informed — and speedier — decisions for wound management and for administering antibiotics.
Because increased water vapor, CO2 and VOCs are associated with bacterial growth and delayed healing, monitoring these factors can help caregivers detect infections earlier and with more confidence.
“Prescribing antibiotics for wounds can be a bit of a gamble,” said Ameer, who is an expert on regenerative engineering approaches to improve wound healing. “Sometimes it’s hard to tell if a wound is infected or not. By the time it’s obvious, it might be too late, and the patient can develop sepsis, which is incredibly dangerous. To avoid this, physicians prescribe a wide spectrum of antibiotics. That can lead to antibiotic resistance, which is a growing problem in health care. Being able to closely, continuously monitor a wound and prescribe an antibiotic at the earliest sign of infection is an obvious and important interest.”
While continuous monitoring is important for all types of wounds, it is particularly crucial for diabetic patients. Ameer previously has developed various strategies, including antioxidant gels and regenerative bandages, for treating diabetic ulcers. Just two years ago, Ameer teamed up with Rogers to create the first transient electronic bandage, which used electrical stimulation to accelerate wound healing. The new wearable provides yet another tool to help these vulnerable patients avoid risky side-effects.
“Diabetic ulcers are the number one non-traumatic cause of lower limb amputations worldwide,” said Ameer. “Sometimes it might appear that the wound is closing, but the skin barrier function is not quite restored. Our device can precisely measure emitted gases, which provides useful information about the skin barrier function.”
Assessing efficacy of bug repellants, lotions
The innovative new technology not only offers unprecedented insights into wound healing and skin health, it also might pave the way for advances in monitoring the efficacy of bug repellents, skin creams and systemic medications designed to improve skin health.
CO2 and VOCs are the very gases that attract mosquitos and other pests. So, measuring these emissions from the skin could help researchers understand and potentially mitigate mosquito attraction. The new device also could enable dermatologists and their patients to measure how fast lotions and creams penetrate the skin, which could provide insights into skin permeability and barrier function. These data also could help other researchers develop more effective transdermal drug delivery systems, monitor the effects of systemically delivered drugs for skin diseases and evaluate the safety of cosmetics and personal care products.
Next, the Northwestern team plans to refine the device’s capabilities, including adding a sensor to track changes in pH levels and developing gas sensors with increased chemical selectivity for early detection of organ dysfunction and other diseases.
“This unusual wearable platform provides a new way to think about and understand skin health,” Rogers said. “This technology is not just about measuring gases and corresponding characteristics of the skin. It's about predicting overall health, preventing infection and disease and creating a future where personalized care is driven by real-time, non-invasive, continuous health tracking through a new collection of parameters that complement those that can be captured with conventional wearables.”
Reference: Shin J, Song JW, Flavin MT, et al. A non-contact wearable device for monitoring epidermal molecular flux. Nature. 2025;640(8058):375-383. doi: 10.1038/s41586-025-08825-2
This article has been republished from the following materials. Note: material may have been edited for length and content. For further information, please contact the cited source. Our press release publishing policy can be accessed here. This Wearable Device Monitors Health by Sensing the Gases Passing Through Your Skin | Technology Networks

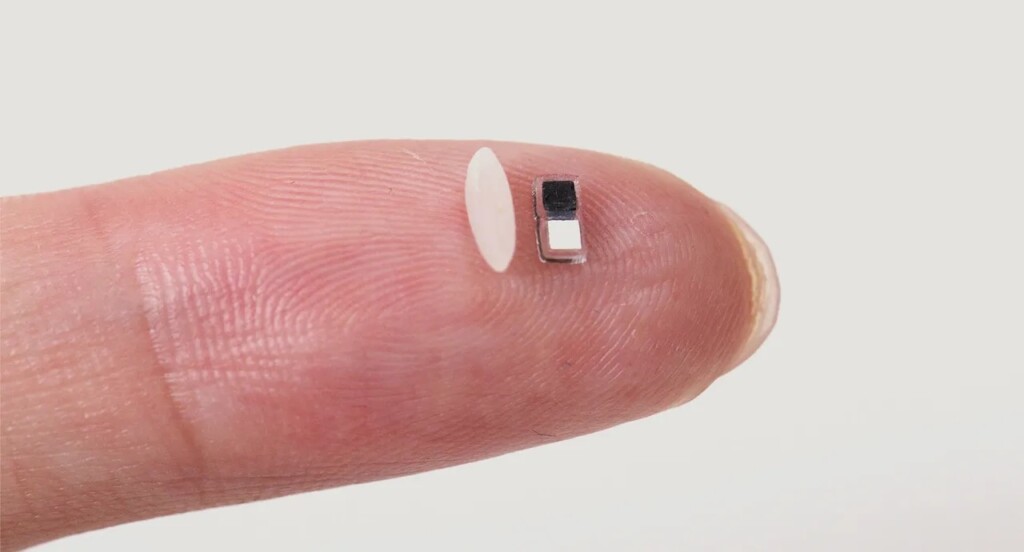 World’s smallest pacemaker next to a grain of rice – Credit: John Rogers / Northwestern University press release
World’s smallest pacemaker next to a grain of rice – Credit: John Rogers / Northwestern University press release